2277
Diagnosis, Characterization of Fetal Sacrococcygeal Teratomas (Type IV) with Prenatal MRI and Its Outcome1Shandong Medical Imaging Research Institute, Shandong University, Jinan, China, China, 2MR Collaboration, Siemens Healthcare Ltd., Beijing, China, China
Synopsis
This study investigated the prenatal diagnosis and prognosis of fetal sacrococcygeal teratomas (SCTs) (Type IV) with Prenatal MRI. Sixteen fetuses with suspected Type IV teratomas were included and followed up in this study. The results showed that prenatal MRI could effectly diagnosed fetal Type IV SCTs, which have a bright outcomes postnatally after surgery resection. This suggests correct diagnosis of teratoma on prenatal MRI and early operation after birth are important for prognosis.
Introduction
Sacrococcygeal teratoma (SCT) is a tumor that occurs in approximately 1 in 35,000 to 40,000 live birth [1]. According to the American Academy of Pediatrics Surgical Section (AAPSS), SCT was described as types I through IV with regard to their location[2]. Most common postnatal SCTs are types I and II, and easily identified after birth. However, the type IV tumors are often recognized several months after birth when they lead to symptoms of constipation and/ or urinary retention, and thus have a higher likelihood of malignant degeneration. So far, no literature has reported the prenatal diagnosis and prognosis of type IV SCTs. Thus, The purpose of this study was to determine the diagnosis, characterization of fetal sacrococcygeal teratomas (SCTs) (Type IV) with prenatal MRI and its outcome.Materials and Methods
This retrospective study was approved by the local ethics review board; written consent was obtained from all subjects. Thirty pregnant women with fetal sacrococcygeal teratoma underwent prenatal MRI (mean age, 35 years ) between Dec.2015 and Nov. 2019. The MRI examinations were performed on a 1.5T MAGNETOM Amira (Siemens, Shenzhen Magnetic Resonance, Ltd., Shenzhen, China) with an 18-channel spine coil and a 13-channels body coil positioned over the lower pelvic area. Susceptibility-weighted imaging (SWI), T2-Weighted Imaging (T2WI), T1-Weighted Imaging (T1WI), Diffusion Weighted Imaging (DWI) were obtained in axial, coronal, and sagittal plane. The size, mass characteristics, and compressive effects of the tumors were determined and correlated with fetal MRI and postnatal findings.Results
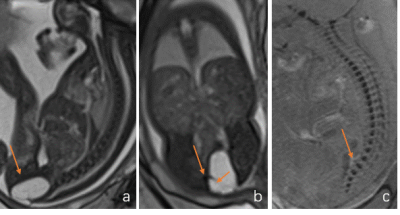
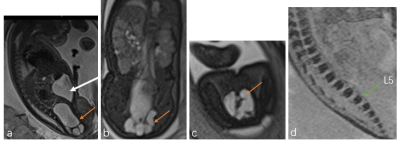
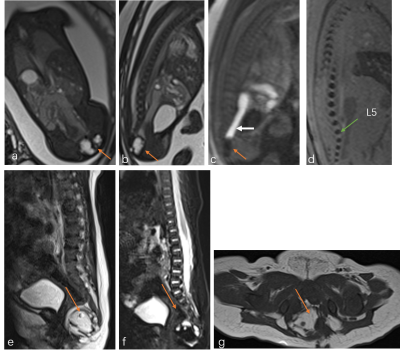
In total, based on the MRI findings, sixteen type IV SCT fetus (mean age, 30 weeks) were enrolled in this study. The diagnosis of sacrococcygeal teratoma was accurate in all cases assessed at our center using prenatal MRI and were confirmed at surgery. The SCT appeared entirely cystic in thirteen fetuses (macrocystic with a few septa in two (Fig 1), microcystic in nine (Fig 2)), mixed cystic and solid in two (Fig 3), and solid in one (fig 4). The mean sizes of the SCTs were 1.8±0.5 cm. Signs of oppression of adjacent rectum and bladder can be seen (fig 2-4). All fetuses underwent MRI and surgical excision within 2 months after birth. All the infants recovered well after surgery except the solid one, with high AFP values. Fetuses with predominantly solid and highly vascularized masses have a poorer prognosis than fetuses with tumors that are mainly cystic and avascular in appearance.Discussion
In previous studies, type IV SCTs usually have poor prognosis because it is usually discovered too late to miss the best time for surgery or local compression effects resulting from a marked increase in tumor size. In our study, all type IV SCTs were correctly diagnosed in prenatal MRI. Signs of oppression of adjacent rectum and bladder can be seen but not leads to secondary effects such as bladder outlet obstruction, hydronephrosis, rectal atresia, sacral bony abnormality, or fetal cardiac failure. Children have an excellent prognosis after early surgical resection in our study. Therefor, prompt diagnosis and resection are critical because the risk of malig-nancy increases with delayedresection.Conclusion
Type IV SCTs could be diagnosed accurately with the prenatal MRI, and have an excellent prognosis after early surgical resection.Acknowledgements
No acknowledgement found.References
[1] Holzgreve W, Miny P, Anderson R, Golbus MS. Experience with 8 cases of prenatally diagnosed sacrococcygeal teratomas. Fetal Ther. 1987;2(2):88-94. doi:10.1159/000263289
[2] Altman RP, Randolph JG, Lilly JR. Sacrococcygeal teratoma: American Academy of Pediatrics Surgical Section Survey-1973. J Pediatr Surg. 1974;9(3):389-398. doi:10.1016/s0022-3468(74)80297-6
Figures